OXA-48-Mediated Ceftazidime-Avibactam Resistance Is Associated with Evolutionary Trade-Offs.
Frohlich, C., Sorum, V., Thomassen, A.M., Johnsen, P.J., Leiros, H.S., Samuelsen, O.(2019) mSphere 4
- PubMed: 30918055
- DOI: https://doi.org/10.1128/mSphere.00024-19
- Primary Citation of Related Structures:
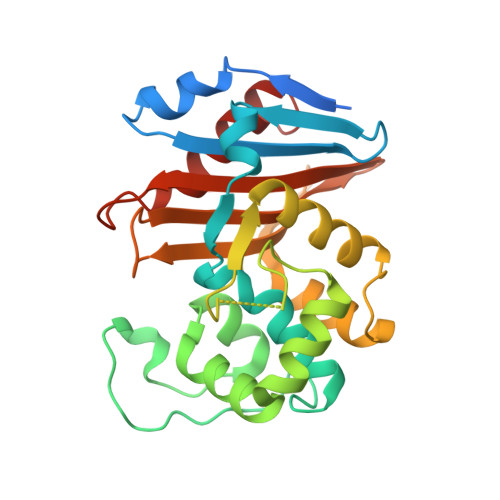
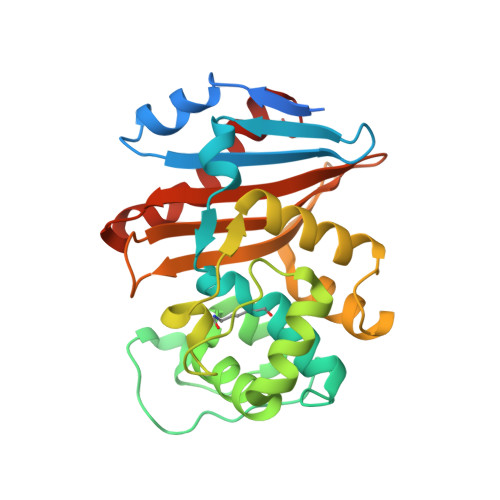
6Q5B, 6Q5F - PubMed Abstract:
Infections due to carbapenemase-producing Gram-negative pathogens are associated with limited treatment options and consequently lead to increased mortality and morbidity. In response, combinations of existing β-lactams and novel β-lactamase inhibitors, such as ceftazidime-avibactam (CAZ-AVI), have been developed as alternative treatment options. To understand the development of resistance and evolutionary trajectories under CAZ-AVI exposure, we studied the effects of ceftazidime (CAZ) and CAZ-AVI on the carbapenemase OXA-48 and the epidemic OXA-48 plasmid in Escherichia coli Exposure of CAZ and CAZ-AVI resulted in single (P68A) and double (P68A,Y211S) amino acid substitutions in OXA-48, respectively. The antimicrobial susceptibility data and enzyme kinetics showed that the P68A substitution was responsible for an increased activity toward CAZ, whereas P68A,Y211S led to a decrease in the inhibitory activity of AVI. X-ray crystallography and molecular modeling of the mutants demonstrated increased flexibility within the active site, which could explain the elevated CAZ hydrolysis and reduced inhibitory activity of AVI. Interestingly, these substitutions resulted in collateral effects compromising the activity of OXA-48 toward carbapenems and penicillins. Moreover, exposure to CAZ-AVI selected for mutations within the OXA-48-encoding plasmid that severely reduced fitness in the absence of antimicrobial selection. These evolutionary trade-offs may contribute to limit the evolution of OXA-48-mediated CAZ and CAZ-AVI resistance, as well as potentially resensitize isolates toward other therapeutic alternatives. IMPORTANCE The recent introduction of novel β-lactam/β-lactamase inhibitor combinations like ceftazidime-avibactam has increased our ability to treat infections caused by multidrug-resistant Gram-negative bacteria, including carbapenemase-producing Enterobacterales However, the increasing number of cases of reported resistance to ceftazidime-avibactam is a concern. OXA-48 is a carbapenemase that has no significant effect on ceftazidime, but is inhibited by avibactam. Since isolates with OXA-48 frequently harbor extended-spectrum β-lactamases that are inhibited by avibactam, it is likely that ceftazidime-avibactam will be used to treat infections caused by OXA-48-producing Enterobacterales. Our data show that exposure to ceftazidime-avibactam can lead to changes in OXA-48, resulting in increased ability to hydrolyze ceftazidime and withstand the inhibitory effect of avibactam. Thus, resistance toward ceftazidime-avibactam among OXA-48-producing Enterobacterales should be monitored. Interestingly, the compromising effect of the amino acid substitutions in OXA-48 on other β-lactams and the effect of ceftazidime-avibactam exposure on the epidemic OXA-48 plasmid indicate that the evolution of ceftazidime-avibactam resistance comes with collateral effects.
Organizational Affiliation:
The Norwegian Structural Biology Centre (NorStruct), Department of Chemistry, UiT-The Arctic University of Norway, Tromsø, Norway [email protected] [email protected].